Preparing for the future with PCMH: The shift from quantity to quality
I am fortunate to be the director of quality improvement with The Compliance Team (TCT). I have been in this role for about 16 months. For 15 years prior to joining TCT, I held numerous nursing and clinic titles with a critical access hospital in Arkansas that had 12 RHCs in Missouri. During my last eight years there, I had the privilege of being one of the RHC clinic administrators with a focus on quality and accreditation.
Starting my nursing career in the hospital setting, I truly had no grasp on how RHCs operated. Unfortunately, hospitals and clinics function in silos – or at least that is how it felt as I was jumping from one silo to the other. I knew nothing about RHC regulations, all-inclusive rates, cost reports, or value-based care. I just thought patients came to the doctor when they had a sore throat or needed refills on medications – so clearly I had a lot to learn.
 |
I was tasked with overseeing a department that hadn’t been developed yet. We were calling it our integrated care department, and it would be responsible for activities with our patients that would lead to improved outcomes through care coordination and community resources. The main programs I would oversee would be chronic are management and a program developed by Missouri Medicaid called the primary care health home (PCHH).
Becoming part of the Missouri PCHH program was not simple, especially for our RHCs. In fact, at the beginning, RHCs were not invited to participate, but our CEO did an excellent job advocating and got that changed. One of the requirements for participation was PCMH accreditation. Once we were accepted into the program, we could begin enrolling patients who were Medicaid beneficiaries and had chronic medical and/or behavioral health diagnoses. We would manage their care utilizing RNs, behavioral health consultants, and community health workers, surrounding them with a care team in close collaboration with their primary care provider. For each patient enrolled in this program, we were paid a set amount per member per month. It was an excellent resource, not only for the patients but for our organization. Being able to fund these services for our patients was going to be a game changer.
 |
My priority was PCMH. I knew very little about this and was thrilled to learn that The Compliance Team offered an accreditation program that would sit nicely atop our RHC accreditation with them. It was an excellent experience with knowledgeable advisors to help along the way.
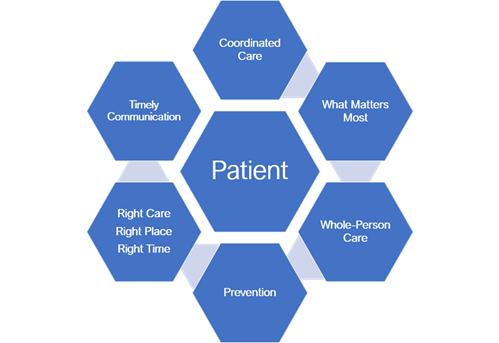
A patient-centered medical home is a model designed to deliver value-based care and allow providers to facilitate wellness at a lower cost, which will make the organization more successful when participating in new and future programs. It puts patients at the forefront and builds better relationships within their care teams. Patients in a PCMH are treated from a whole-person perspective to help them access care and resources that might not otherwise be addressed in a traditional primary care setting. Accreditation provides structure and accountability while fostering an environment of quality improvement. PCMH principles are based on enhancing day-to-day operations to improve patient access and strengthen care coordination activities to bridge gaps in health care delivery.
Change is challenging, but the transformation I witnessed within the clinics and our patients’ lives was undeniable. The focus shifted from illness to wellness. We were having discussions about prevention at each visit. We were assessing for barriers, such as social determinants of health, and offering resources. We made efforts to identify patients frequently accessing the ER and work with them to establish action plans. Patients started chattering within the community about the “extras” their doctor’s offices were doing for them. Staff were feeling more invested, and patients were becoming more engaged. It was a true culture shift.
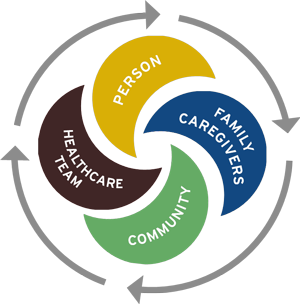 |
It wasn’t easy, but we knew it was a crucial steppingstone to keep up with the direction health care was headed. Value-based care, also known as accountable care, is ultimately designed to improve patient satisfaction and outcomes while financially rewarding providers for the quality of care they are providing at a lower cost. By prioritizing quality over quantity, health care can be more effective and efficient. According to HHS, the goal is for all Medicare beneficiaries and a vast majority of Medicaid beneficiaries to be in an accountable care relationship by the year 2030. That is just around the corner, but it seems like many are wondering how and where to start. The key is prevention and proactive care utilizing a team-based approach with high-level care coordination between transitions, and ensuring patients have access to their primary care team when they need it. The key is becoming a patient-centered medical home.
Within just a couple of years of becoming a PCMH, our chronic care management program had grown from 100 to approximately 1,500 patients and our efforts were being rewarded within our ACO. Other payers were inviting us to participate in financially rewarding incentive programs. Our volume had increased due to a focus on capturing annual wellness visits, and our star ratings significantly improved. We never looked back.
Testimonials from other TCT PCMH accredited clinics highlight many of the benefits.
| “Being an accredited patient-centered medical home has put the patient at the very core of our practices. While seeing our patients, we have improved workflows to look at all aspects of the patient’s health, not just their chief complaint for that visit. We are ensuring that they have established goals, have enhanced after-hours access to their health care providers, are closing their open care gap opportunities, and are receiving the best quality of care. Since being accredited, we’ve noticed that our quality scores have increased, and patient satisfaction has increased as well.” |
| “We don’t receive nearly the amount of calls or complaints we used to receive regarding patients wanting their test results. It feels like the provider teams are really tuned into their patients’ care and working with them to close the care gaps. Things just run smoother between the patient and the provider.” |
The Compliance Team is one of only five accreditation organizations nationally recognized by CMS to accredit clinics for PCMH and is advantageous for RHCs in many ways. When the outcome matters, the method must be achievable. How is your clinic going to achieve this innovative milestone?
NRHA adapted the above piece from The Compliance Team, a trusted NRHA partner, for publication within the Association’s Rural Health Voices blog.
