Thinking differently: Staffing and retaining your surgeons and anesthesiologists
First, we need to ensure our surgical departments are adequately staffed. Second, we need to rethink how we staff and manage our surgical departments, especially when it comes to on-call duties. Thankfully, there is a solution that helps hospitals and health care systems address these issues in a more strategic and effective way.
Where have all the doctors gone?
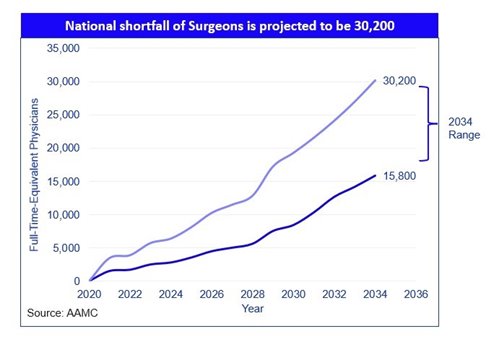
From a practical standpoint, a number of factors are impacting physician retention and patients’ access to care, both now and in the future. One is a surge in demand: 10,000 Baby Boomers are turning 65 every day, which is increasing demand for age-related services such as orthopedic surgeries. Meanwhile, doctors themselves are aging, and there is a shortage of medical school graduates to fill their roles. According to the Association of American Medical Colleges (AAMC), in less than 10 years there could be a shortfall of more than 30,000 surgeons.
 |
Additionally, our health care system is still feeling the impact of the COVID-19 pandemic. Not only did the pandemic leave patients with more complex health care needs, it left doctors feeling burned out and disillusioned. The rate of suicide among physicians is staggeringly high, above that of even combat veterans. According to the American Medical Association, record numbers of doctors are leaving or planning to leave their profession at a time when we need them most.
For nearly every hospital, surgery is one of the top specialties that drives the most revenue. However, without a fully staffed surgical team that includes qualified surgeons, anesthesiologists, and advanced practitioners, hospitals are not able to meet patient demand for care and fill their surgical blocks. These factors are contributing to many hospitals experiencing declining revenues and cutting services while worsening the health care professional shortage in our country.
Along with the administrative burdens physicians face running their practice and the strain of on-call duty, these pressures are driving doctors out of the profession. According to AAMC data,25 percent of physicians have made plans for early retirement. Of those not leaving, one-third would like to reduce their work hours at a time when demand is rising.
How to staff up and rethink on-call duties
When physicians are burned out by the demands of on-call duties on top of their normal administrative requirements and in-clinic hours, this leads to a reduction in the number of hours they’re able to work. In turn, this creates longer wait times for appointments or procedures, resulting in care delays and negatively impacting patient experience.
Innovative solutions for rural hospitals and practices
There is a solution to this issue that enables hospitals to staff adequately, manage their programs effectively, and build centers of excellence while allowing doctors to live their best lives professionally and personally. It’s called the surgicalist model, and it’s already being used by hospitals nationwide.
Under this model, “surgicalist” surgeons – as well as anesthesiologists and other advanced practice professionals – work pre-set shifts supporting hospital emergency on-call needs or covering full surgical departments. This specialized model gives the surgicalist the flexibility to work seven to 10 consecutive days per month, allowing for predictable blocks of time off. It also allows the private practice surgeons they are supporting to care for their patients with limited or no emergency department on-call responsibilities, eliminating care conflict. Because they have the support of surgicalist doctors who cover on-call shifts, private practice surgeons in a hospital system or other health care practice can take time off, leave work at work, and return refreshed for the next day’s patients.
Surgicalists function as a clinical team (usually a team of three), all of whom are assigned coordinated shifts covering emergency department on-call needs or supporting a full surgical program for emergent, elective, and inpatient consult needs. Surgicalist teams work coordinated shifts 24/7/365 with detailed handoffs. Unlike locum tenens physicians, surgicalists are dedicated to their hospital facility, serve on committees, engage with the community, and work side by side with the hospital’s other staff as a true team member.
This model delivers major benefits to hospitals, including decreased patient wait times and length of hospital stays; improved patient throughput; increased elective surgery volume; increased downstream revenue; increased surgical volume within emergency departments; decreased transfers out of the facility; decreased time between ER and OR admittance for patients needing surgery; improved HCAHPS survey ratings indicating higher patient satisfaction; and a decrease in unnecessary patient readmissions.
Hospitals and health care organizations, even in difficult-to-staff areas like rural regions and certain metropolitan locations, benefit from a fully staffed surgicalist model. One rural hospital system in West Virginia that employed the surgicalist model to establish, develop, staff, and grow an orthopedic surgery program has reported that its surgeons have achieved 90 percent or higher patient satisfaction and have supported a 40 percent increase in patient volume, allowing more patients to get the care they need locally instead traveling long distances.
It is time for us to take action to change our health care system in a way that makes surgeons and anesthesiologists want to stay in the profession and provide their vitally needed skills to the patients and facilities that desperately need them. Staffing and managing these clinicians in a way that helps all doctors live their best lives improves the lives of patients, which is the ultimate goal.
NRHA adapted the above piece for publication within the Association’s Rural Health Voices written by Dr. Richard Makowiec, MD, MBA, an orthopedic surgeon and chief surgical officer of Synergy Health Partners, a trusted NRHA partner.
